By Scott Finkernagel, Senior Biosafety Manager
Antibiotic resistance is one of the greatest concerns for the healthcare industry and public health. Antibiotics and antifungals (both types of antimicrobials) save lives, but any time they are used—for people, animals, or plants—they can contribute to resistance. In 2021, the CDC reported that U.S. hospitals saw significantly higher rates for four out of six types of healthcare-associated infections (HAIs). Many of these HAIs are resistant to antibiotics or antifungals.
As attention to antibiotic-resistant organisms increases, many in the professional cleaning space have begun to question whether pathogens can also develop resistance to chemical disinfectants. Disinfectants are used to reduce the concentration of pathogenic microorganisms to a safe level and help to prevent the transmission of infectious diseases. However, there is confusion around this question as there are actually two types of pathogen resistance:
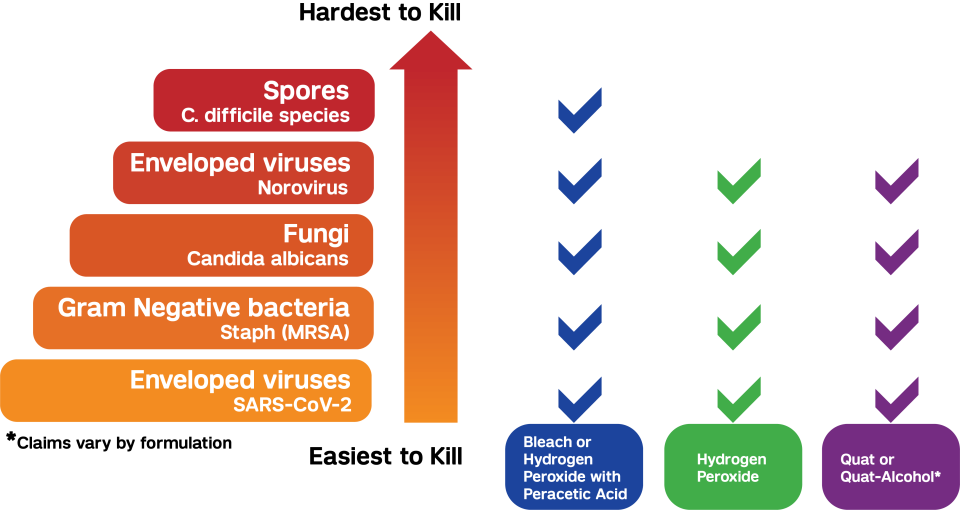
1. Innate resistance – Pathogens vary significantly in their natural resistance or susceptibility to antimicrobials and chemical disinfectants (i.e., how easily are they killed by antimicrobials or disinfectants). For example, spores are highly resistant to disinfectants and, therefore, hardest to kill because of their spore coat and outer shell, which act as a natural barrier. This is not something that is acquired or changes over time. The pathogen hierarchy chart below helps to demonstrate the innate resistance of varying pathogens to the various chemical disinfectants available today.
2. Acquired resistance – Acquired resistance happens when pathogens, like bacteria and fungi, develop the ability to defeat the drugs designed to kill them. This often happens due to the selective pressure that occurs when antimicrobials are used to kill germs that cause infections, but they fail to kill all the remaining pathogens because some have natural immunity. The antimicrobial-resistant germs survive and multiply.
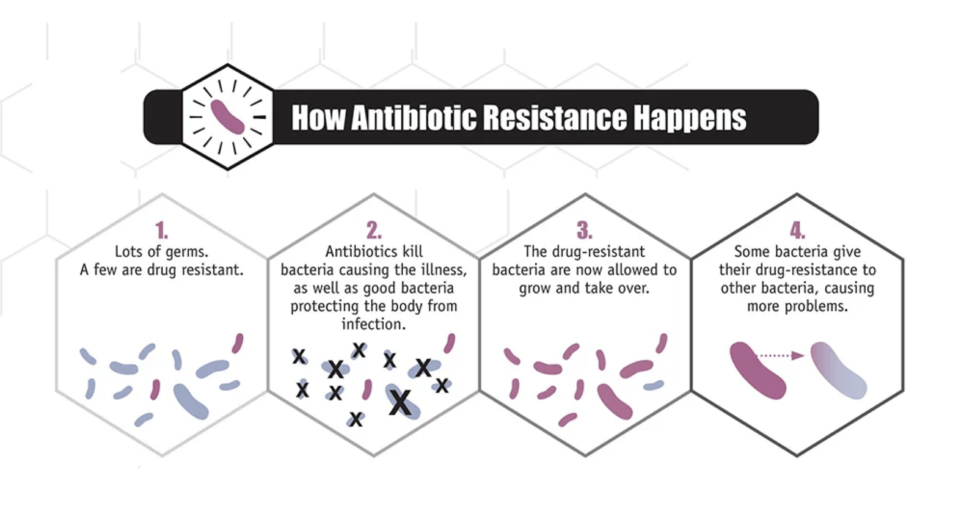
Pathogens can acquire resistance to disinfectants when used improperly. Disinfectants can impart selective pressure on some types of bacteria, resulting in the development of acquired resistance. However, bacteria can only develop resistance to certain types of disinfectants if the concentration of the active ingredient is too low to be efficacious. This can occur from human error while mixing, storing, and handling dilutable disinfectants, or when the product label directions for use are not followed correctly (contact time, expiry date, etc.).
While research on disinfectant resistance is ongoing, one thing is clear: pathogens do not become resistant to disinfectants or germicides in the same way they do to antimicrobials. Notable differences include, but are not limited to:
Disinfectants have multiple ways of attacking pathogens. In fact, the method of kill is entirely dependent on the active ingredient(s) and how they are formulated. In general, disinfectants can denature, oxidize, or attack pathogens in various ways.
Disinfectants are used on inanimate surfaces rather than inside the body. By contrast, antimicrobials are used inside the body and, therefore, have limitations on the overall concentration that can be used safely inside a human body. This allows disinfectants to be used at concentrations far exceeding the required minimum kill concentration (known as the minimum inhibitory concentration). Therefore, a small increase in resistance, while critically important to an antimicrobial, would be of little relevance to the effectiveness of a disinfectant.
If a facility uses good quality U.S. EPA-registered disinfectants and uses them correctly, there should be no concerns about disinfectant resistance. Disinfectants are one of the most viable protections against multi-drug- resistant organisms. Consider the following factors when selecting the right disinfectant:
Review the organisms and pathogens being handled and their susceptibility to the proposed disinfectant.
Compatibility of the disinfectant and surfaces that will need to be disinfected.
Required concentration and contact time to achieve disinfection.
Product preparation, shelf life, and storage.
Appropriate personal protective equipment, as many chemical disinfectants are respiratory, skin, and eye irritants.
References

